I don’t have diabetes, but I wore an implant that measures the sugar in my blood to see if I could hack my performance. I’d put it back on again if I could.
- For 20 days this fall, I wore a device that tracks my blood sugar in real time, in the hope that it would help me find ways to boost my performance and energy through changes to my diet and exercise.
- The device I wore, a Dexcom G6, is a prescription device typically used by those living with diabetes. But it’s gained increasing popularity among “biohackers” in Silicon Valley who have hopes of using the data to improve their performance.
- While it was exciting to learn which foods sent my blood sugar soaring and which didn’t, I mostly found out that in fact my body processes blood sugar the way it’s supposed to when working out or after a big meal.
- I still learned a lot about my body, and by the end, I was bummed I had to take it off.
For a few weeks this fall, I had a pretty good idea of what was going on in my pancreas at any given time.
That’s because I was wearing a continuous glucose monitor, or CGM. The device uses a wire inserted into my skin to get an idea of the amount of blood sugar, or glucose, found in my blood.
It’s a prescription device typically used by people managing diabetes, both Type 1 and Type 2, conditions in which it’s harder to regulate the amount of blood sugar present in the body.
For those managing diabetes, checking on blood sugar levels is an important part of managing the condition, and it can be done either with periodic glucose meter readings taken by finger prick or with continuous monitors like those made by Dexcom, Abbott, or Medtronic.
The one I tested out: A Dexcom G6, a version of Dexcom’s CGM that got approved in March 2018.
To be sure, I’m not the intended user of a CGM.
“Ultimately, the whole goal is to prevent low blood sugars and to ensure that you can prevent low blood sugars while achieving glycemic control,” Dr. Adrian Vella, an endocrinologist at the Mayo Clinic in Rochester, Minnesota told me.
That’s important if you’re managing diabetes. The device hasn’t been studied for use in people who don’t have diabetes.
“There’s no data to guide us on how to use it in a healthy person,” Vella said.
But for years, I’d been eager to see what I could learn from tracking my blood sugar as a person who isn’t living with diabetes.
I’ve tried a number of stress trackers and put on my fair share of step, sleep, and heart-rate tracking devices. Each time I took off a device I was reviewing or testing, I didn’t feel a burning desire to put it back on.
But my blood sugar levels, I thought, might reveal more information that could help me hack my diet, exercise routines, and hopefully energy levels. And I’m not the only one – Silicon Valley biohackers have also been keen users of the technology in the hopes of improving their performance.
What I learned wasn’t exactly the case. While it was exciting to see which foods sent my blood sugar soaring and which didn’t, I mostly found out that in fact my body processes blood sugar the way it’s supposed to when working out or after a big meal.
Even so, I was addicted to checking out my blood sugar levels while wearing it, and oddly miss it now that I’ve used up my sensors.
Here’s what it was like to use.
First, a little about me: I’m a 26-year-old who doesn’t have diabetes. I just spent the past few months training for the New York City Marathon, a race I ran with my dad (pictured).

I’ve been covering diabetes closely over the past few years, in particular because of the issues around the skyrocketing cost of insulin, a drug used to help those living with diabetes process the blood sugar in their bodies. The 1.25 million people in the US who have Type 1 diabetes need to inject insulin to live.

Through my reporting, I’ve heard a lot about CGMs, or continuous glucose monitors, a device many living with type 1 and type 2 diabetes use to help them manage the conditions.

I’d also spoken with a number of people who don’t have diabetes who had worn the devices for periods of time. They told me anecdotal incidents of how using the device changed their eating habits in particular. Seeing the spike in blood sugar for instance after eating a bagel swore them off the delicious carbohydrate-loaded bake.
So when I was offered the chance to try one myself, I jumped at it. Dexcom sent me its G6 device to test out. It came with a device that would implant my sensor, a device that’d pick up readings from that sensor, and an optional monitor I could use to see whether my blood sugar was going up or down. I instead opted to use my phone. I was given two sensors, and each would last me 10 days.

At first, I was a little daunted by all the equipment, so I recruited my colleague Rachel Gillett, who has type 1 diabetes and has been my in-office CGM expert, to help walk me through it. I downloaded the app, watched some training videos, and figured out where I wanted my sensor to go.

Before I could put it on, I needed to link the sensor up with my phone by scanning a code on the back.

Next, I pulled off the top layer, exposing the adhesive surface I’d place against my skin.

With Rachel’s help, I lined it up on the back of my arm.

…and with a click of a button on the top, a needle pierced my arm, leaving behind a wire that would keep an eye on my blood sugar levels. In less than a second, the needle was out of my arm.

Next, I slid in the transmitter that would help the sensor communicate with my phone. My sensor would expire after 10 days, but the transmitter can be used with more than one sensor, so I had to be sure to keep it when getting rid of the sensor.

Just like that, I was ready to go. The sensor took a few hours to calibrate, and once it was all set up, it told me that my blood sugar was dangerously low. With Rachel’s help, I checked my blood sugar using a finger-prick and used that information to calibrate my CGM.
When I was done, I had to throw the plastic applicator in the trash. Dexcom CEO Kevin Sayer said that while there isn’t a recycling program in place now, the company will create one, and it’s also working to make the device smaller, or potentially reusable.
With that, I was off and running. I didn’t feel the CGM very much after the first day, only remembering it when I’d accidentally snag it when getting dressed.

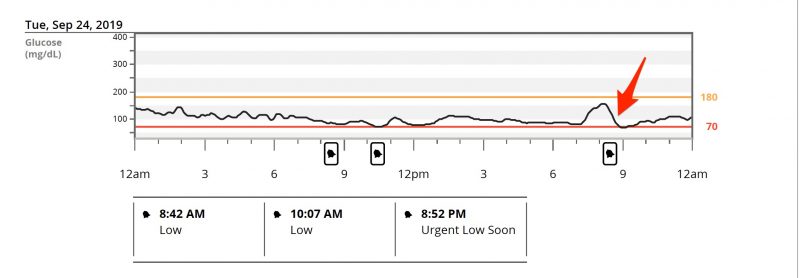
The first week, I kept my diet pretty standard: I typically have a banana in the morning, snacks or a meal around noon, and then I try to eat a full meal around 7 p.m. in the evening. On my second day, I had a beer with my meal at one of my favorite barbecue restaurants and was surprised to find that my blood sugar levels fell like crazy. Here’s a look at the moment my blood sugar fell after my beer.
Alcohol has a curious effect on blood sugar levels.
I would have thought that my blood sugar spiked, giving the carbohydrates in beer. But it turns out there’s a “decreased endogenous glucose production” after drinking alcohol, a fancy way of saying that my body wasn’t making as much blood sugar in reaction to the alcohol in my system.
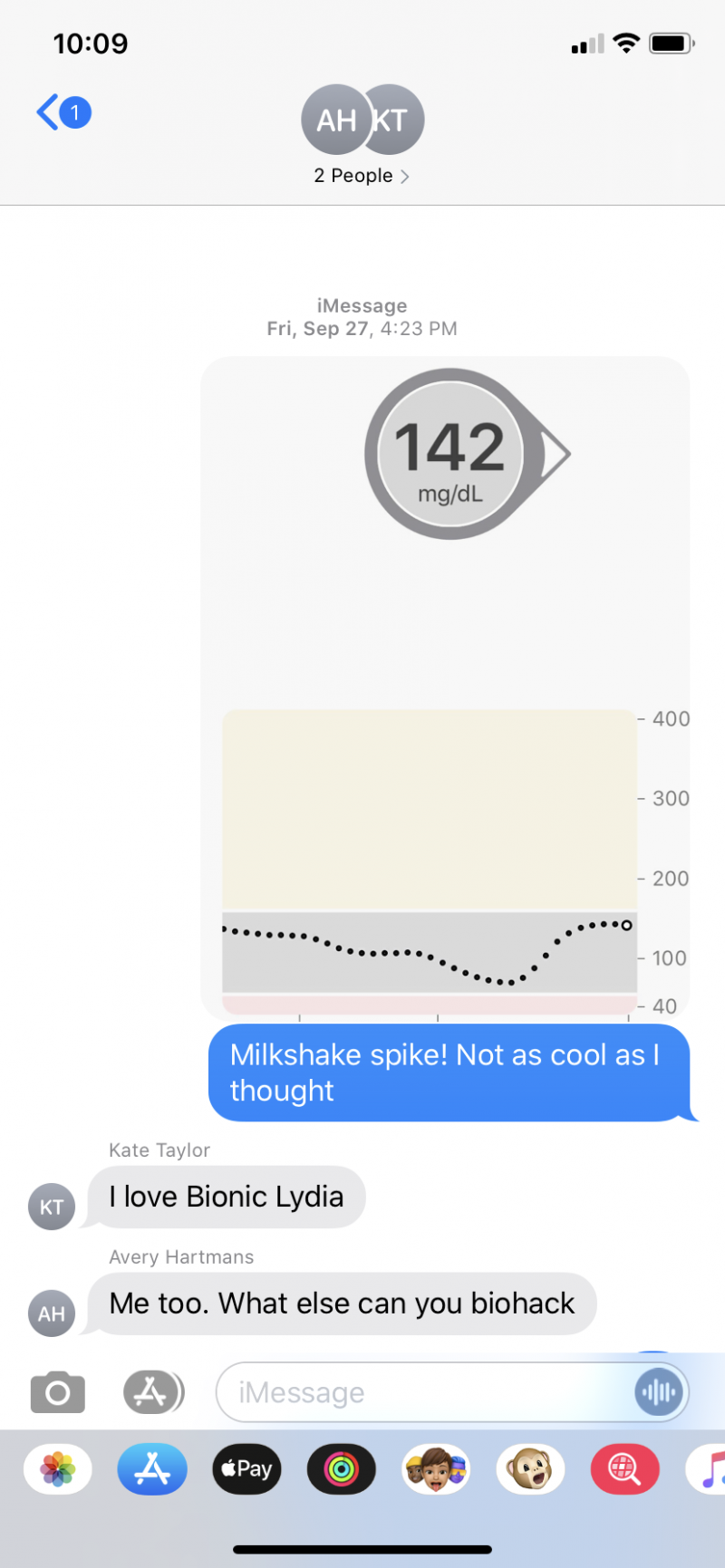
I was curious to see what other foods might send my blood sugar levels spiking or crashing, so a few days later I convinced some of my colleagues to join me for an afternoon milkshake run.

Eager to show them what I learned, I texted them a screenshot of my post-milkshake spike. Even if I was a bit underwhelmed, it was still cool to see the reaction.
I spoke with Henrik Berggren, the cofounder and CEO of Steady Health, a startup that’s building a tech-enabled clinic for diabetes care. Berggren himself has type 1 diabetes and has been using a CGM. He passed along the advice that the interesting insights from CGMs come when you start to compare responses, rather than seeing what ice cream can do to your system like I did.
“You already know those things are bad for you,” Berggren said.
The more interesting observations come in quantifying what I have worse reactions to (in this case, dramatic spikes in blood sugar levels) compared to others.
Take breakfast – what would a banana do to my blood sugar compared with a granola bar, compared to fasting until noon? Over the next few weeks, I’d do a bit of that, but not enough to make me change my morning eating habits.
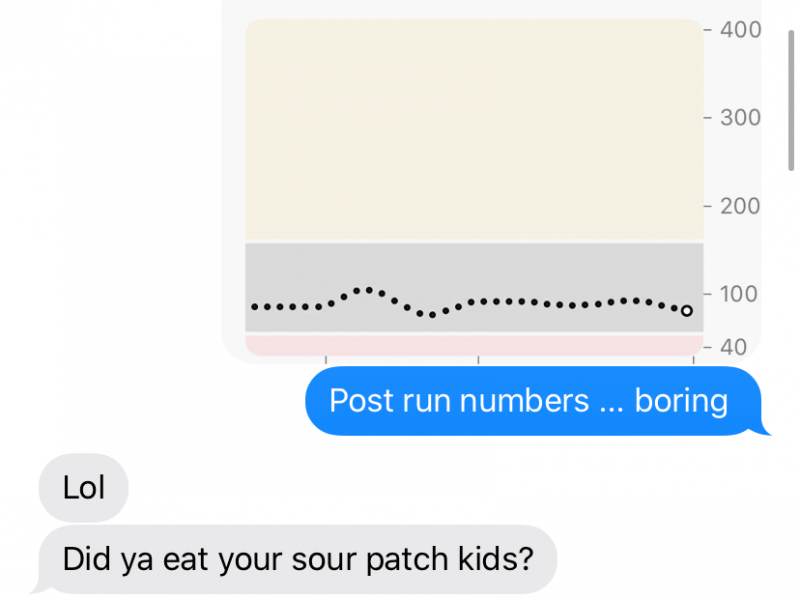
But it wasn’t just reactions to food I was eager to learn more about. I had a marathon coming up after all, and I was curious if I could use my blood sugar readings from the CGM to boost my energy in moments when I was feeling low. On a long run that weekend, I packed some Sour Patch Kids for instant hits of sugar. Whenever I noticed my blood sugar was dipping lower, I ate a few gummies.

But at the end of 11 miles, I wasn’t able to boost my blood sugar levels in any meaningful way. I texted my husband a snapshot of my results with my disappointment.
The way our bodies react to exercise can differ, even between activities.
Berggren said he found that when he wore a CGM he learned a lot more about how his body reacts to certain types of exercise, which helps him better administer insulin that keeps his blood sugar from going too high.
For instance, compared to activities like running, an activity like basketball would make his blood sugar spike, so he learned to take more ahead of getting onto the court.
I thought I could ascribe my 3 p.m. energy slump to crashing blood sugar levels. But when I’d look at my blood sugar levels, they’d be holding steady after my body was done processing my lunch. (Even so, I’d often give myself the excuse to go for an afternoon snack).
Turns out, the body is more complicated than I had initially thought. Blood sugar levels don’t exactly correlate to energy levels.
There are other factors, like caffeine intake, hormones, how well I slept the night before, how hydrated I am, and general feelings of procrastination, that could contribute to my afternoon slump.
And even in cases when my blood sugar stays low, like while running long distances, it doesn’t mean I’m out of fuel.
“I like to tell patients that the body is like a hybrid car,” Vella said. Using the hybrid analogy, Vella explained that you can either run the body on gas or electric (in our case carbohydrates or fat). So just because your blood sugar is low doesn’t mean your body is out of energy.
I noticed some interesting changes in my blood sugar while I was sleeping. About the time I’d go to bed, my blood sugar would creep up (promise I wasn’t sneaking any late night snacks). I also saw a little pick-up in my blood sugar level around 3 a.m. — a well-known phenomena known as the “Dawn Effect.”
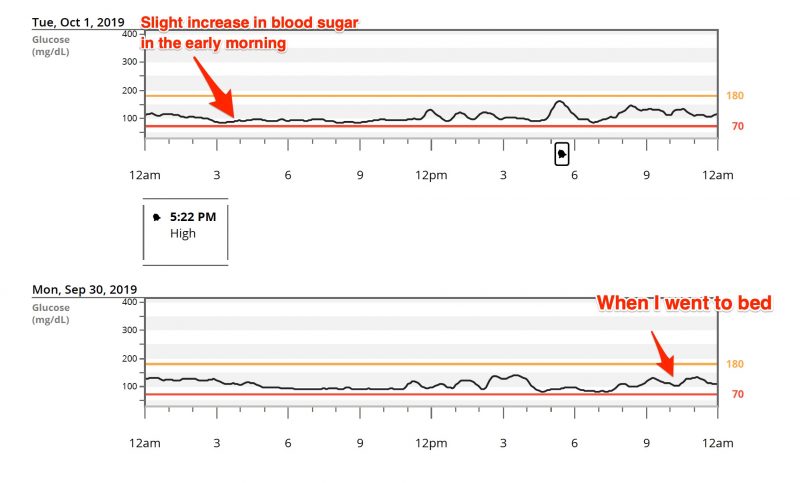
Source: Mayo Clinic
Before I knew it, my sensor was about to expire. It had been fun to wear. I got some odd looks when people saw it, and once a man stopped me excitedly on the subway to ask if it was “the new Fitbit.” When I explained it was tracking my blood sugar, he was apologetic (understandable, as it’s typically used in a medical context and isn’t a consumer health gadget).

I put on another one a few days before the marathon, this time opting to put it on my stomach (the place Dexcom recommends placing it). I found it a little trickier to maneuver with high-waisted jeans, but I didn’t snag it as much as when I had it on my arm.

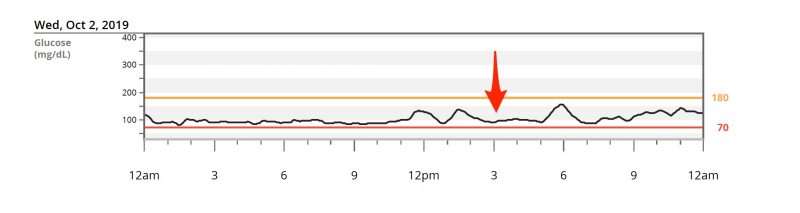
The day of the marathon, I was eager to see what might happen with my blood sugar levels. That morning in Staten Island, I ate a bagel, drank coffee, and had a banana (the first spike of the day). Later, I nervously ate a Stroopwafel (the second spike). That incredibly flat line starting around 10:30 is from while I was running. I had thought the Gatorade I had grabbed every two miles or so would send my blood sugar spiking, but it didn’t appear to make any difference.
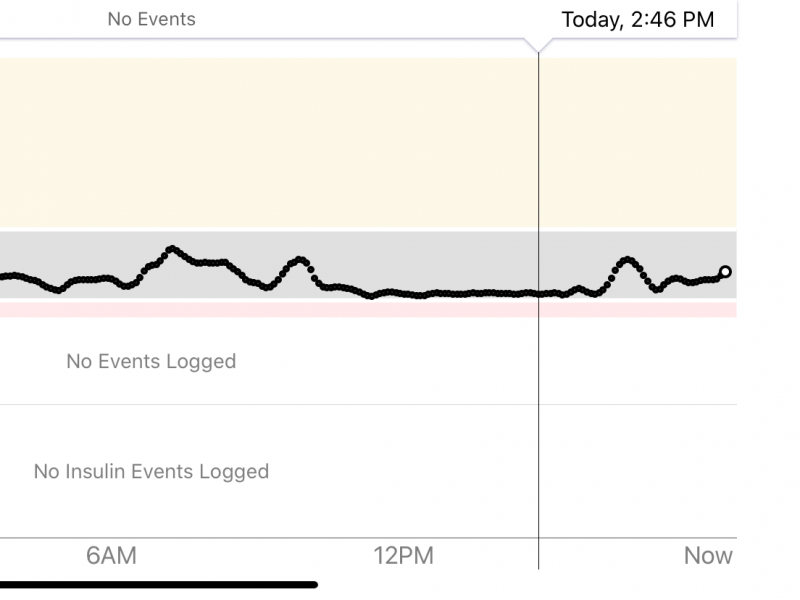
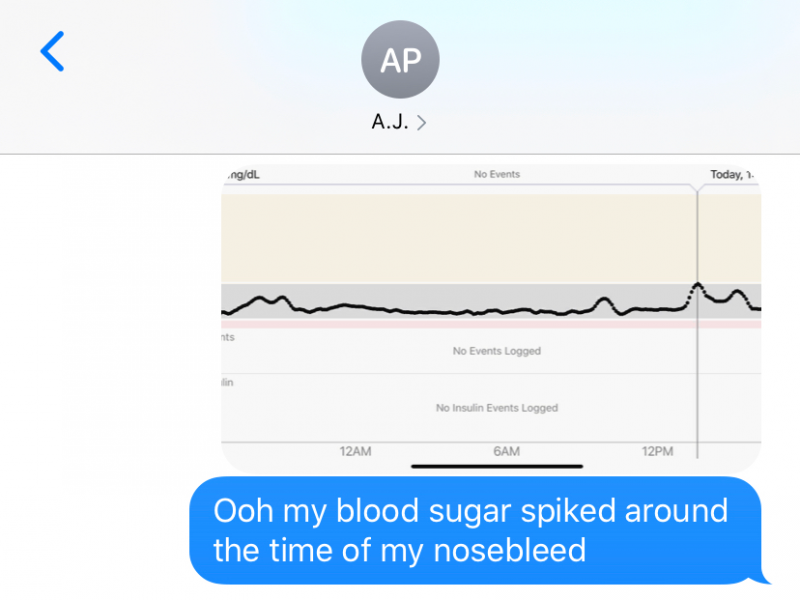
After the marathon, I still had my CGM on, and I noticed a big spike in my blood sugar around the same time my nose spontaneously started bleeding (in the middle of some breaking news if you can believe it!)
After I took off my second sensor, I looked back at the data I collected.
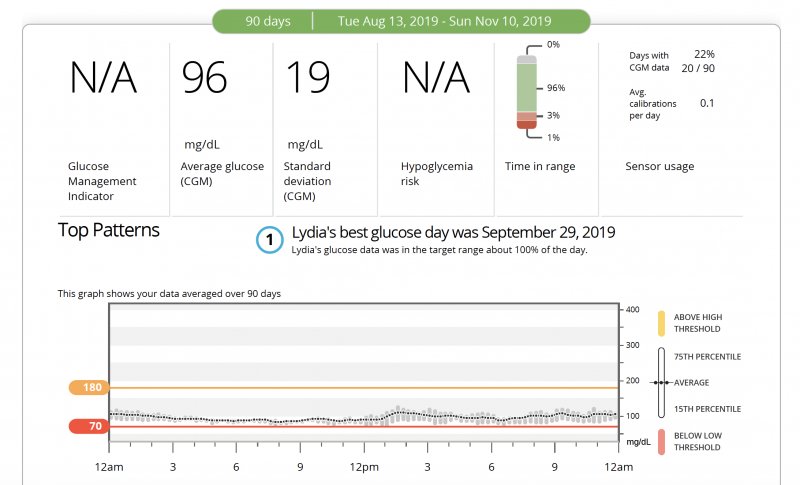
On the whole, my numbers looked pretty good. I hadn’t experienced too many crazy big changes in my blood sugar and stayed pretty consistent day after day.
At the end, though, what I found myself taking away from the experience was that my pancreas was working just as it should.
Vella, the endocrinologist, told me that it may not be particularly useful information for healthy people like me if outside a study. While someone living with type 1 might find out what insulin dose they should administer before a workout with the help of a CGM, my takeaways weren’t as clear cut.
Even so, some doctors have found a use for it in their clinical work.
“For me it’s a wonderful tool to make sense of the puzzle,” said Dr. George Haddad, the chief medical officer of the P4 Medicine Institute in Seattle.
As he brings on new patients in his practice, he’ll give them a CGM to wear, which helps him better understand how their body reacts to carbohydrates.
Still, if I could’ve put in another sensor, I would’ve. I would love to test out the differences in my blood sugar levels while training and while not training. I never got a chance to see what happens when I eat Chinese takeout, which I’m told can send blood sugar levels soaring.

At the same time, I won’t miss worrying about where my blood sugar is at any given moment. I’d be alerted if my blood sugar fell below the parameters I had set on the app. The alerts would get pretty annoying, and I’d find myself giving myself the excuse to have a little snack just to stop the alerts, even though I inherently knew they weren’t a problem.
Much like checking a social media app, I found myself constantly opening my Dexcom app to see where my numbers were, thinking through if there was anything I needed to do about them, which, of course, wasn’t necessary.
My blood sugar had behaved that way before I put on the device and would continue to after I took it off. When I’m not wearing the device, I don’t have that concern on my brain at all.
While I’d imagine the main uses for CGMs will continue to be in managing diabetes, with some popularity among the Silicon Valley biohacking crowd, I’ll be curious if there’s a world in which glucose monitoring becomes more popular among people without diabetes.
It’ll likely take more research in people who don’t have diabetes, and potentially even less-invasive options that resemble a step or sleep tracker with no needles involved.
A true love for health

Recent Comments